Health Professionals
On this page you will find news, data, and interesting information from and for the Health Care Provider. Click on a link and enjoy!
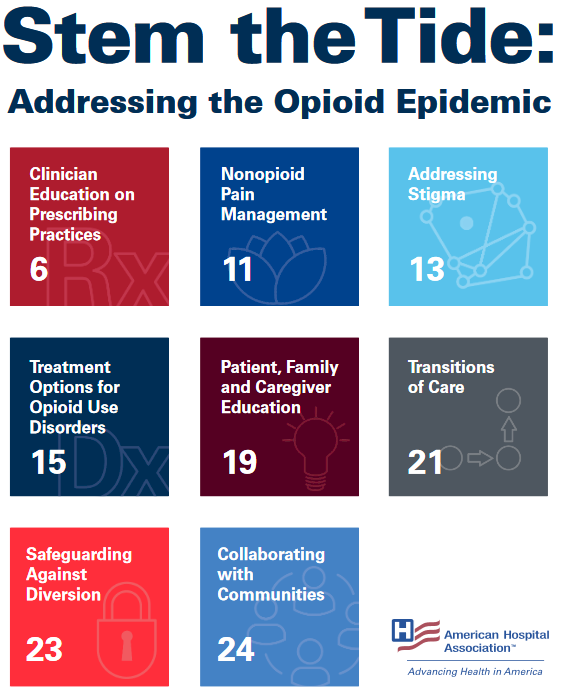
Stem the Tide: Addressing the Opioid Epidemic by the American Hospital Association
Every day, hospitals and health systems see the effects of the nation’s opioid epidemic. According to the Centers for Disease Control and Prevention, more than 33,000 people died from an opioid-related overdose in 2015. That’s more than 90 people a day or approximately four people each hour. There are also financial implications due to increased health care and substance use disorder treatment costs, lost productivity and costs to the criminal justice system, estimated to be $78.5 billion in 2016.
This toolkit includes resources for hospitals and health systems to share with clinicians and patients and to use to enhance part-nerships within their communities. The information is categorized into eight topic areas:
1. Clinician education on prescribing practices
2. Nonopioid pain management
3. Addressing stigma
4. Treatment options for opioid use disorders
5. Patient, family and caregiver education
6. Transitions of care
7. Safeguarding against diversion
8. Collaborating with communities
Each topic area includes a variety of resources, national and state guidelines, training, simulations and case examples. The AHA recognizes that hospitals and health systems must tailor their efforts to meet the resource realities and unique needs of their local communities. Click Here to learn more.
Physician Continuing Education to Reduce Opioid Misuse, Abuse and Overdose - Many opportunities and Few Requirements
Physician continuing education to reduce opioid misuse, abuse, and overdose are sorely needed across the country without many opportunities to receive training and few requirements to do so. Please Click Here to read an article on physician continuing education to reduce opioid misuse, abuse and overdose. This article focuses on the opioid overdose epidemic in the United States being driven in large part by inappropriate opioid prescribing. Most American physicians receive little or no training during medical school regarding best practice prescribing, substance use disorders, and pain management. There are very few states that require continuing medical education (CME) on these topics. This article reports the results of a systematic legal analysis of physician training requirements, together with recommendations for improved physician training and much more.
Here is the full link to the article; https://www.researchgate.net/publication/301759691_Physician_continuing_education_to_reduce_opioid_misuse_abuse_and_overdose_Many_opportunities_few_requirements
Medical Association of Georgia Foundation (MAGF), Dr. Tennent Slack, M.D, “The Prescription Opioid Overdose Epidemic - A Question of Balance”
Dr. Tennent Slack, MD, a pain physician in Gainesville, Georgia and co-chair of MAGF’s "Think About It" campaign, presents "The Prescription Drug Overdose Epidemic -- A Question of Balance." In this presentation, Dr. Slack defines the scope of the prescription drug overdose crisis; discusses why the problem has occurred and the difficulty in effectively addressing it. In closing, he outlines how the Medical Association of Georgia Foundation's Think About It campaign is focused on reducing prescription drug abuse.
To view this powerful insightful presentation please Click Here (https://www.youtube.com/watch?v=ue2IhUWkZFI).

Steven J. Stack, MD
Immediate Past President American Medical Association

A call to action: Physicians must turn the tide of the opioid epidemic
We have a defining moment before us—the kind of moment that we will look back on in years to come as one in which we as a profession rose to the challenge to save our patients, our families and our communities during a time of crisis.
Our nation is needlessly losing thousands of people to a preventable epidemic, and we must take action for our patients.
A time for action
Over the past 15 years, the nation’s opioid epidemic has claimed more than 250,000 lives, according to data from the Centers for Disease Control and Prevention (CDC). In the last year alone, we lost nearly 30,000 friends, neighbors, children and spouses.
Those numbers are alarming—and they require swift intervention.
In fact, there’s something of a parallel with what we’re seeing now and the early years of the HIV/AIDS epidemic. Nearly 320,000 people died in the first 15 years of that epidemic.
Thankfully, the narrative doesn’t end there. The nation’s policymakers, public health leaders and physicians came together to implement solutions that changed the course of history for people with an HIV/AIDS diagnosis and their loved ones.
It’s time to mount a similar response for the opioid epidemic. The loss of lives we are seeing around us and in the news every day is unacceptable—and we don’t have to accept it. Each and every one of us must band together to take specific actions that will turn the tide.
What we need to do
It’s time to mount a similar response for the opioid epidemic. The loss of lives we are seeing around us and in the news every day is unacceptable—and we don’t have to accept it. Each and every one of us must band together to take specific actions that will turn the tide.
One of the great hallmarks of our profession is to run toward an emergency, to stand with our patients in the midst of their most pressing needs and to show the nation a clear path forward.
One way that our profession has done that for the opioid epidemic so far has been to convene a task force with more than 20 state and specialty medical associations, the American Osteopathic Association and the American Dental Association to identify best practices and implement them across the country.
For us as individuals, there are five specific steps we all must take:
- We should register for and use our state’s prescription drug monitoring program (PDMP) if we treat patients for pain, mental illness or any other condition for which a controlled substance could be prescribed. Not every PDMP is perfect, but they provide important information that can help us when considering whether to prescribe a controlled substance for a particular patient.
- We may need to enhance our education and training about safe prescribing. There are significant barriers to providing non-opioid and non-pharmacologic treatment alternatives, but we should ask ourselves two simple questions: When was the last time we looked at the research on opioid alternatives? And when was the last time we took education to ensure we are prescribing safely and appropriately? The AMA has gathered more than 100 state and specialty-specific education resources in a one-stop shop for the best and most up-to-date education that organized medicine has to offer. Be sure to take advantage of these materials.
- We should co-prescribe naloxone to patients at risk of overdose. The overdose reversal drug naloxone has saved more than 26,000 lives in the community in recent years, according to the CDC. The AMA Task Force to Reduce Prescription Opioid Abuse offers concrete recommendations for when you should consider co-prescribing naloxone to your patients.
- We should get training to provide medication-assisted treatment (MAT) for substance use disorders. More of us need to be trained to recognize patients with substance use disorder, and more physicians need to become certified to increase access to treatment. Several medical organizations offer waiver-qualifying MAT training in multiple formats.
- We need to speak out against stigma and stand up for what we know is right. Patients in pain deserve care and compassion, not judgment. Treating pain is among the most difficult—and most common—reasons patients come to us. As physicians, we are often under pressure to “satisfy a patient’s pain.” Sometimes this requires prescribing an opioid. But caring also means sometimes saying no and recommending an alternative course of treatment—no matter how difficult that may be.
Our nation’s opioid epidemic won’t end unless we become leaders by supporting the necessary policies and making the necessary practice changes. I urge you to join me in taking these steps today. Now is the time to act—this is our moment to turn the tide.